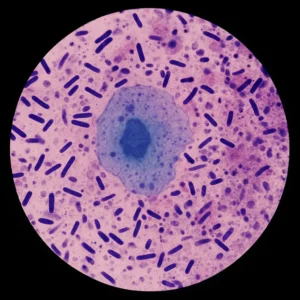
The vaginal microbiome and hormonal health are intricately connected, forming a dynamic relationship where each can influence the other. This interplay impacts various aspects of health, from reproductive function to systemic hormone balance.
- Chronic Inflammation & Stress
- Inflammation – chronic inflammation caused by vaginal dsybiosis can lead to hormone disruption. Inflammatory cytokines can interfere with hormones including cortisol, insulin and oestrogen, which can contribute to hormonal imbalances.
- Role in the Stress Response – the vaginal microbiome plays a role in your immune system and function, which influences the HPA axis, a key regulator of the stress response and hormones.
2. Oestrogen Regulation
- The Oestrobolome – the is most commonly studied in the gut, however the oestrobolome relates to specific bacteria that regulate oestrogen levels (via producing specific enzymes). Therefore dsybiosis in microbiomes such as the gut microbiome or vaginal microbiome, can potentially alter oestrogen metabolism and disrupt hormonal health.
- Oestrogen Metabolism – the microbiome interacts with oestrogen, therefore dsybiosis here can negatively impact this and disrupt hormonal health.
- Supporting Lactobacillus growth – Oestrogen aids in producing glycogen, which is the main food source of Lactobacillus species. These species are the ‘good’ bacteria in your microbiome and promote a healthy microbiome balance.
3. Menstrual Cycle Impact
- Stabilising of Cycles – a balanced microbiome helps to regulate the fluctuations in sex hormones (like oestrogen and progesterone), that occur during the menstrual cycle. In comparison and imbalanced microbiome may contribute to irregular menstrual cycles, which are linked to hormonal imbalances.
4. Infection Risk
- Your vaginal microbiome influences your susceptibility to infections such as BV, UTIs, STIs, and thrush. Chronic infections can disrupt hormonal balance, contribute to inflammation and negatively impact your health. A balanced vaginal microbiome protects against infections and limits your risk of such.
Link to Specific Conditions
- PCOS – those with PCOS are less likely to have Lactobacillus species dominance, and are more likely to have vaginal dsybiosis. This dsybiosis may play a role in further exacerbating hormonal disruptions, such as higher androgens and irregular ovulation.
- Endometriosis – chronic inflammation is a hallmark of Endometriosis. Vaginal microbiome imbalance contributes to chronic inflammation and can therefore worsen the effects of Endometriosis. There is increasing research investigating the role of specific bacterial species’ potential role in Endometriosis, such as Fuseobacterium.
How ScreenMe can help you to improve & optimise your vaginal microbiome health:
- Education: Our site, Instagram, Spotify and Youtube are filled with resources to help you learn how to improve your intimate health!
- Testing: ScreenMe offers the gold-standard, NGS testing, which allows for 100% of the bacteria in your microbiome to be screened with 99.9% accuracy. This allows you to fully understand the context of your microbiome, and address your concerns.
- Support: All tests come with a free 1:1 consultation with an intimate health expert, who will talk you through your results and create a bespoke plan of action for you. Therefore you are empowered to make the decisions that are right for you and your body.
Conclusion:
The vaginal microbiome is deeply intertwined with hormonal health, playing a vital role in maintaining reproductive, immune, and systemic balance. Disruptions to this delicate ecosystem can contribute to or exacerbate hormonal imbalances, highlighting the importance of nurturing microbiome health for overall well-being.
Fariba Khonsari